Neurofeedback therapy targets the symptoms of tinnitus by aiming to regulate and optimize the brainwave patterns associated with the condition. Specifically, it focuses on addressing the overactivity or irregular patterns in the auditory and sensory processing areas of the brain that may contribute to tinnitus symptoms. By providing real-time feedback to the patient about their brainwave activity, neurofeedback helps them learn to self-regulate and modify these patterns, potentially reducing the perception and impact of tinnitus.
Muscle TensionIn tinnitus patients, neurofeedback aims to address specific brainwave patterns such as increased delta and theta activity, as well as irregularities in the alpha and beta frequencies. By training the brain to modulate these patterns, neurofeedback seeks to promote greater stability and balance in the neural activity associated with tinnitus, potentially leading to symptom improvement.
NeurofeedbackNeurofeedback can be used as a standalone treatment for tinnitus, but it is often integrated with other therapies for a comprehensive approach. Combining neurofeedback with techniques such as sound therapy, counseling, or relaxation exercises may enhance the overall effectiveness of tinnitus management, addressing both the neurological and psychological aspects of the condition.
Delta Waves
While neurofeedback therapy has shown promise in addressing various types of tinnitus, research suggests that certain subtypes, such as somatic tinnitus, may particularly benefit from this approach. Somatic tinnitus, which is linked to muscular or vascular factors, may respond well to neurofeedback due to its focus on regulating neural activity and addressing underlying physiological contributors.
The typical duration and frequency of neurofeedback sessions for tinnitus management can vary based on individual needs and treatment plans. However, many patients undergo multiple sessions per week over several months to achieve optimal results. The duration of each session may range from 30 to 60 minutes, with the overall treatment course tailored to the patient's progress and response to neurofeedback.
Galvanic Skin Response Biofeedback
Neurofeedback therapy for tinnitus generally has minimal side effects and is considered safe for most individuals. Data Acquisition However, it may not be suitable for those with certain neurological conditions, such as epilepsy, or individuals who are unable to participate actively in the training process. As with any treatment, it's essential for patients to consult with qualified healthcare professionals to determine the appropriateness of neurofeedback for their specific circumstances.
When comparing neurofeedback to other non-invasive treatments for tinnitus, such as sound therapy or cognitive behavioral therapy, it's important to recognize that each approach offers unique benefits. While sound therapy aims to provide relief by masking tinnitus sounds, and cognitive behavioral therapy focuses on changing the emotional and behavioral responses to tinnitus, neurofeedback directly targets the underlying neural activity associated with the condition. Integrating these approaches based on individual needs and preferences may offer a comprehensive and personalized strategy for tinnitus management.
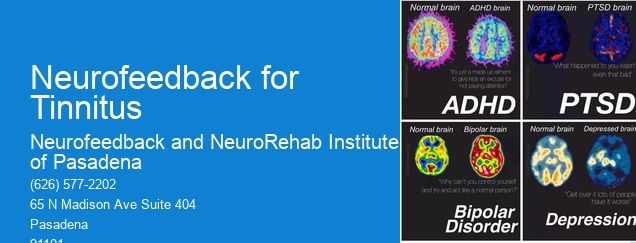
Neurofeedback approaches for addressing treatment-resistant depression may include techniques such as electroencephalography (EEG) biofeedback, neurostimulation, and real-time functional magnetic resonance imaging (rtfMRI) neurofeedback. These approaches aim to modulate brain activity and regulate neural networks associated with mood regulation, emotional processing, and cognitive function. Additionally, protocols involving alpha-theta training, sensorimotor rhythm (SMR) training, and low-frequency repetitive transcranial magnetic stimulation (rTMS) may be utilized to target specific brain regions and neural oscillations implicated in depression. Furthermore, personalized neurofeedback protocols tailored to individual neurophysiological patterns and symptom profiles may be employed to enhance treatment efficacy and address the unique neurobiological underpinnings of treatment-resistant depression.
Neurofeedback for postpartum depression during breastfeeding presents unique challenges due to the need to consider the impact of the treatment on both the mother and the infant. The practitioner must carefully monitor the effects of neurofeedback on the mother's mental health while ensuring that it does not interfere with breastfeeding or affect the infant's well-being. Factors such as hormone levels, sleep patterns, and stress management become crucial in tailoring the neurofeedback protocol to address the specific needs of the postpartum mother. Additionally, the practitioner may need to collaborate with lactation consultants and mental health professionals to provide comprehensive support for the mother's overall well-being. It is essential to approach neurofeedback for postpartum depression during breastfeeding with a holistic understanding of the interconnectedness of the mother-infant dyad and the specific challenges it presents.
Yes, there are specialized neurofeedback protocols designed specifically for Parkinson's disease patients. These protocols often focus on targeting the specific neural pathways and brain regions affected by Parkinson's disease, such as the basal ganglia and motor cortex. Neurofeedback training for Parkinson's disease may involve protocols that aim to improve motor function, reduce tremors, enhance cognitive function, and address non-motor symptoms such as depression and anxiety. These protocols may utilize techniques such as sensorimotor rhythm (SMR) training, beta training, and coherence training to address the unique neurological challenges presented by Parkinson's disease. Additionally, personalized neurofeedback protocols may be tailored to the individual needs and symptoms of each Parkinson's disease patient, taking into account factors such as disease progression, medication effects, and comorbidities.
Neurofeedback therapy targets specific phobias such as claustrophobia by utilizing real-time monitoring of brainwave activity to provide feedback and training to the individual. Through the use of specialized equipment, the therapy aims to regulate and optimize brain function, addressing the underlying neural patterns associated with the phobia. By employing techniques such as operant conditioning and neuroplasticity, neurofeedback therapy seeks to retrain the brain's response to triggers related to claustrophobia, promoting a more adaptive and less fear-driven reaction. This process involves identifying and addressing specific neural pathways and patterns associated with the phobia, ultimately leading to a reduction in the individual's fear response and an improved ability to cope with enclosed spaces.
Neurofeedback therapy, also known as EEG biofeedback, has shown promise in the management of postpartum depression. This non-invasive treatment modality involves training individuals to regulate their brainwave activity, which can help alleviate symptoms of depression, anxiety, and stress. By providing real-time feedback on brainwave patterns, neurofeedback aims to promote self-regulation and improve emotional well-being. Research suggests that neurofeedback may be beneficial in addressing the emotional and cognitive challenges associated with postpartum depression, offering a potential adjunct or alternative to traditional interventions. While further studies are needed to establish its efficacy in this specific context, neurofeedback therapy holds potential as a complementary approach to postpartum depression management.
When parents are considering neurofeedback as a treatment option for their children with ADHD, there are several important considerations to keep in mind. It's crucial for parents to thoroughly research and understand the process of neurofeedback, including how it works, potential benefits, and any associated risks. They should also consult with healthcare professionals, such as pediatricians, neurologists, or psychologists, to gain a comprehensive understanding of the treatment and its suitability for their child. Additionally, parents should consider the commitment required for neurofeedback therapy, as it often involves multiple sessions over an extended period. It's important for parents to have realistic expectations about the potential outcomes of neurofeedback and to be prepared to actively participate in their child's treatment process. Furthermore, they should explore the financial implications and insurance coverage for neurofeedback therapy, as well as the availability of qualified and experienced practitioners in their area. Lastly, parents should consider their child's individual needs, preferences, and comfort level with the treatment approach, and ensure open communication with their child throughout the decision-making process.
The age of onset and severity of Tourette's syndrome can significantly impact the outcomes of neurofeedback interventions. Research suggests that early intervention, particularly during childhood or adolescence, may lead to more favorable results in managing Tourette's symptoms through neurofeedback. Additionally, individuals with milder forms of Tourette's may respond more positively to neurofeedback compared to those with more severe symptoms. Factors such as the specific neural pathways affected, the degree of motor and vocal tics, and the presence of comorbid conditions can also influence the effectiveness of neurofeedback in addressing Tourette's syndrome. Understanding the nuanced relationship between age of onset, severity, and neurofeedback outcomes is crucial for tailoring interventions to individual needs and optimizing therapeutic benefits.